Most wildland fire organizations have reduced or eliminated indoor meetings, training sessions, and air travel in order to reduce the spread of COVID-19. Research and real world experiences are coming to light illustrating why this is a good decision.
The COVID-19 virus becomes airborne by talking and can spread through the air staying aloft for 8-14 minutes according to one study, or perhaps for hours according to another. Air conditioning can cause droplets containing the virus to travel around a room. There is much less risk when personnel are outside, since the droplets can be dispersed.
The longer a person is exposed to a contaminated atmosphere, the greater is the risk of introducing more virus than their body can easily handle. A short exposure may have no obvious effect, but if it is longer the disease could gain a foothold that can be difficult or impossible to fight off.
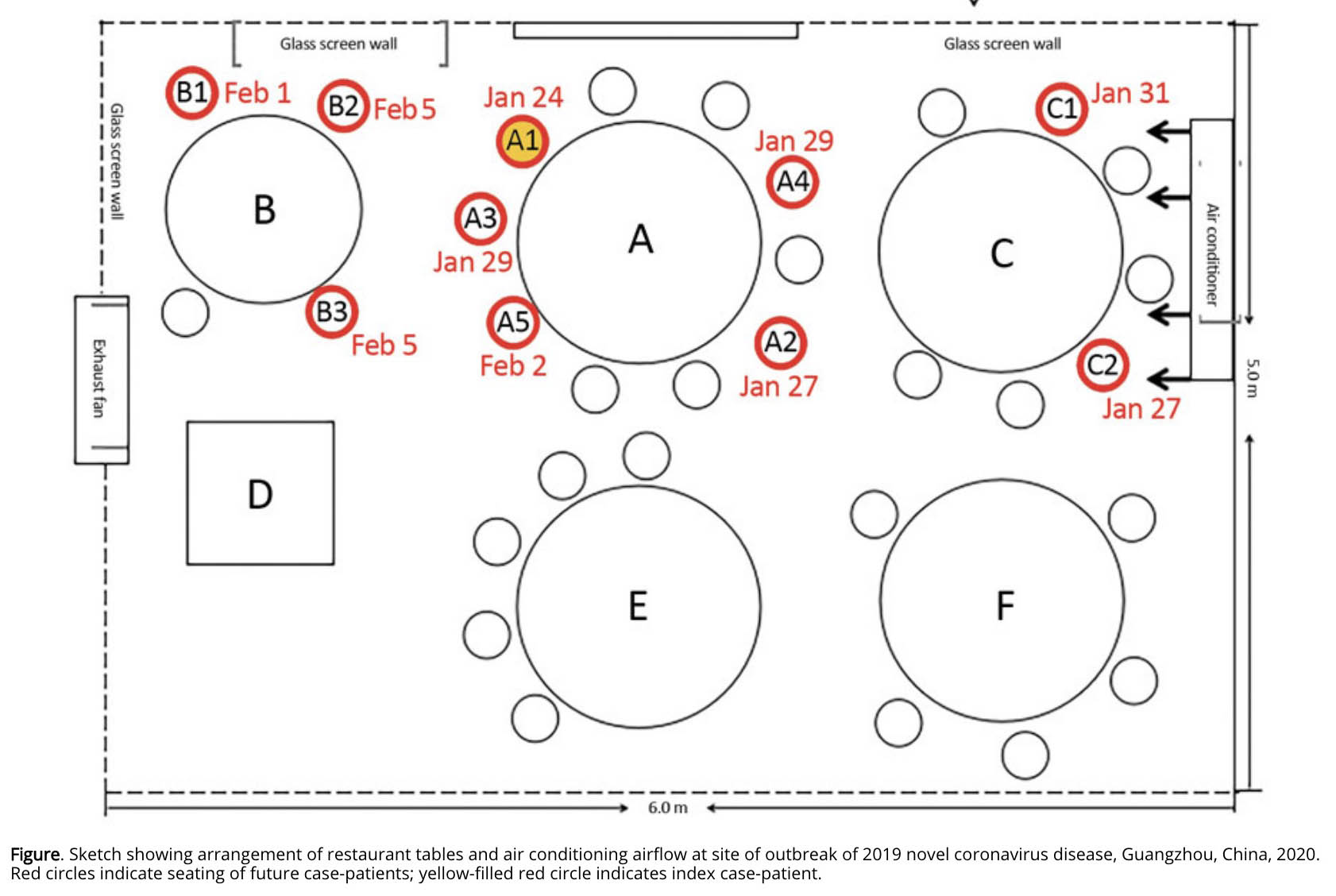
Here is an excerpt from a study published by the U.S. Centers for Disease Control (CDC). The above illustration is from the article.
Abstract
During January 26–February 10, 2020, an outbreak of 2019 novel coronavirus disease in an air-conditioned restaurant in Guangzhou, China, involved 3 family clusters. The airflow direction was consistent with droplet transmission. To prevent the spread of the virus in restaurants, we recommend increasing the distance between tables and improving ventilation.From January 26 through February 10, 2020, an outbreak of 2019 novel coronavirus disease (COVD-19) affected 10 persons from 3 families (families A–C) who had eaten at the same air-conditioned restaurant in Guangzhou, China. One of the families had just traveled from Wuhan, Hubei Province, China. We performed a detailed investigation that linked these 10 cases together. Our study was approved by the Ethics Committee of the Guangzhou Center for Disease Control and Prevention.
On January 23, 2020, family A traveled from Wuhan and arrived in Guangzhou. On January 24, the index case-patient (patient A1) ate lunch with 3 other family members (A2–A4) at restaurant X. Two other families, B and C, sat at neighboring tables at the same restaurant. Later that day, patient A1 experienced onset of fever and cough and went to the hospital. By February 5, a total of 9 others (4 members of family A, 3 members of family B, and 2 members of family C) had become ill with COVID-19.
The only known source of exposure for the affected persons in families B and C was patient A1 at the restaurant. We determined that virus had been transmitted to >1 member of family B and >1 member of family C at the restaurant and that further infections in families B and C resulted from within-family transmission.
A study in the Proceedings of the National Academy of Sciences determined that droplets from speech can stay aloft for 8-14 minutes.
Speech droplets generated by asymptomatic carriers of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are increasingly considered to be a likely mode of disease transmission. Highly sensitive laser light scattering observations have revealed that loud speech can emit thousands of oral fluid droplets per second. These observations confirm that there is a substantial probability that normal speaking causes airborne virus transmission in confined environments.
From an Associated Press article — a different COVID virus in very small aerosols “remained suspended in the air almost indefinitely”.
Since the aerosol particles produced by talking and breathing are so small, they linger in the air for relatively long periods of time before gravity pulls them to the ground. This allows them to be transported over greater distances. A 2006 study of SARS-CoV-1 found that particles with a diameter of 1-3 µm remained suspended in the air almost indefinitely, particles 10 µm in size took 17 minutes, and 20 µm took 4 minutes to fall to the floor. A recent laboratory study found that the virus can remain viable and infectious in aerosols for hours (it remained viable for the entire three-hour duration of the study) and on surfaces for up to days.
And finally, a study published by the CDC about a choir practice in Skagit County, Washington.
Among 61 persons who attended a March 10 choir practice at which one person was known to be symptomatic, 53 cases were identified, including 33 confirmed and 20 probable cases (secondary attack rates of 53.3% among confirmed cases and 86.7% among all cases). Three of the 53 persons who became ill were hospitalized (5.7%), and two died (3.7%). The 2.5-hour singing practice provided several opportunities for droplet and fomite transmission, including members sitting close to one another, sharing snacks, and stacking chairs at the end of the practice. The act of singing, itself, might have contributed to transmission through emission of aerosols, which is affected by loudness of vocalization.
